I’ve felt like a fraud living with IBD for as long as I can remember. Right back to my school days when I used a toilet card to leave class rather than wait for a teacher’s permission (which wasn’t always forthcoming...You’ve been once already, you’re not going again). Then right through to university, when I was given extra time and extenuating circumstances for my exams. Through to full time working life, when things became more difficult and I unconsciously stopped checking in with my needs and started operating on an empty tank.

The hidden nature of IBD makes it so much harder to speak up and to ask for what you need to better your life in school, university and work. The difference with work is that you really have to build your own boundaries and find the confidence to keep them there. Your health will suffer otherwise. It is only now, 10 year into my legal career, that I feel confident enough to identify as disabled in the workplace. And it took major life changing surgery to get me there. But I’m there...FINALLY. And I won’t turn back.
I am done with feeling like a fraud and with trying to justify (or hide...or outright ignore) what I need. I’m done with trying to prove that I’ve earned the little allowances that I get from having a hidden disability. I don’t need to prove how ill or well I am to anybody. Around the time of my stoma surgery, things got darker for me than ever before and since then, I’ve known that I have to do everything I can to avoid going back. That means overcoming my fear of what other people think of me. And healing the part of me that felt like a fraud.
Half the battle of living with an invisible illness like IBD is that nobody can see your internal struggles and the misconceptions about the disease only serve to make things harder. If I had £1 for every time somebody said, “I have IBS, so I know how you feel” my pockets would be a lot heavier! The truth is, IBD is incredibly different to IBS.
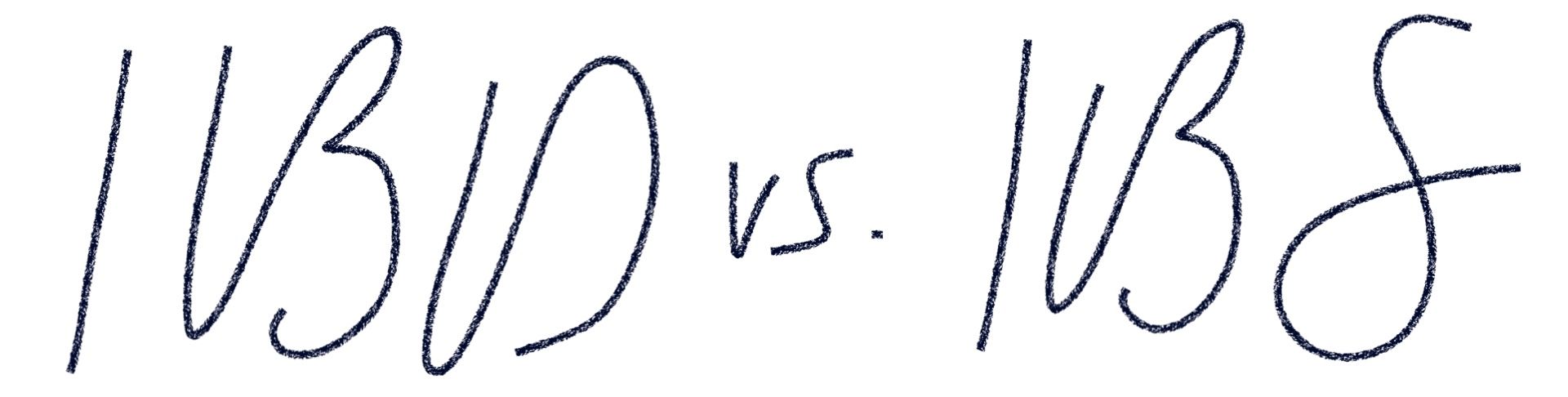
- IBD is a structural autoimmune disease that causes inflammation and ulceration in the GI tract. IBS is a functional syndrome (a group of symptoms) that causes digestive problems and increased gut sensitivity.
- The inflammation and ulceration caused by IBD results in permanent harm to your digestive tract. IBS does not cause any damage to the GI tract.
- To diagnose IBD a doctor will look for physical damage (inflammation or ulceration) in your intestines. Tests will not show any physical reason for your IBS symptoms.
- IBD symptoms can include frequent and/or urgent bowel movements, abdominal pain, diarrhoea, bleeding, weight loss or loss of appetite, fever and inflammation in your skin, joints and/or eyes. IBS symptoms can include bloating, constipation and/or diarrhoea.
- Crohn’s disease usually causes pain the lower right side of your belly and colitis usually causes pain the in the left side. IBS generally causes pain or cramps in the lower half of your abdomen.
- Without treatment, IBD can lead to serious problems such as bone loss, infection, blood clots, a blocked or perforated bowel or rapid widening of your colon. IBS does not carry these risks and is generally seen as being less dangerous.
- IBD is treated with drugs that aim to reduce the inflammation such as steroids, immunosuppressants and biological therapies. Some people with IBD need surgery to repair or remove the damaged part of the GI tract. Those with IBS are treated with symptom specific medications i.e. for diarrhoea or constipation and rarely require hospitalisation or surgery.
- IBD comes with an increased risk of colon cancer. IBS has no associated increased risk of colon cancer.
If you don’t have IBD but you know somebody who does, I am sure it would mean the world if you reached out to say that you are learning more about IBD and how it affects them. To say that you see their internal struggles. That you are not only behind them when they say no if they need to but that you encourage them to take time out. You encourage them to stick to their boundaries. Because that is the kind of support that gives IBD sufferers the confidence to put themselves first and give themselves the best chance of staying well or getting better.
I hope that by continuing to talk about IBD and how it affects me, others in the same situation will feel more empowered to reach out to their loved ones, their friends, their employer to ask for the help they may so desperately need. So that they get to the point I have much quicker than I did. It should not take 10 years. And little by little, through this blog, I hope that I too will get stronger in sticking to those boundaries and in asking for what I need to live my happiest and healthiest life.
Love Me
& My Friend Wendy.


Comments